Fibromyalgia is a complex chronic pain disorder characterized by widespread musculoskeletal pain, fatigue, sleep disturbances, and cognitive difficulties. For many years, the exact mechanisms underlying fibromyalgia have remained elusive, leading to challenges in diagnosis and treatment. However, emerging research has increasingly implicated neuroinflammation—the activation of inflammatory processes in the central nervous system (CNS)—as a key contributor to the pathophysiology of fibromyalgia. In this article, we delve into the latest insights from research on neuroinflammation and its implications for understanding and managing fibromyalgia.
Understanding Fibromyalgia
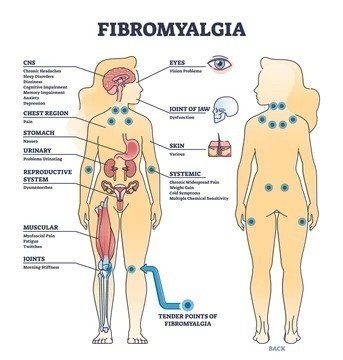
Fibromyalgia affects an estimated 2-8% of the global population, predominantly women, and is characterized by widespread pain and tenderness in muscles, joints, and soft tissues. In addition to pain, individuals with fibromyalgia often experience fatigue, sleep disturbances, cognitive dysfunction (often referred to as “fibro fog”), and mood disturbances such as depression and anxiety. Despite its prevalence and significant impact on quality of life, fibromyalgia remains poorly understood, and effective treatments are limited.
Neuroinflammation and Fibromyalgia
Neuroinflammation refers to the activation of inflammatory processes within the CNS, including the brain and spinal cord. While inflammation is a natural response of the immune system to injury or infection, chronic or dysregulated neuroinflammation can lead to persistent pain and dysfunction in conditions such as fibromyalgia.
Emerging research has provided compelling evidence of neuroinflammatory changes in the brains of individuals with fibromyalgia. Neuroimaging studies using techniques such as positron emission tomography (PET) and functional magnetic resonance imaging (fMRI) have revealed alterations in brain regions involved in pain processing, emotion regulation, and cognitive function. These changes include increased activation of microglia—the primary immune cells of the CNS—and elevated levels of pro-inflammatory cytokines, signaling molecules that promote inflammation.
Furthermore, studies have identified abnormalities in the neuroendocrine and autonomic nervous systems, which play a role in modulating pain perception and stress responses. Dysregulation of these systems may contribute to the development and maintenance of fibromyalgia symptoms, including pain sensitivity and fatigue.
Implications for Treatment
The growing recognition of neuroinflammation in fibromyalgia has significant implications for the development of targeted treatments. While current pharmacological therapies for fibromyalgia primarily focus on symptom management, targeting neuroinflammatory pathways may offer novel therapeutic approaches that address the underlying pathophysiology of the condition.
Several potential strategies for modulating neuroinflammation in fibromyalgia are being investigated, including:
- Anti-inflammatory Agents: Drugs that inhibit pro-inflammatory cytokines or modulate microglial activation represent promising candidates for reducing neuroinflammation and alleviating fibromyalgia symptoms. Clinical trials evaluating the efficacy of anti-inflammatory medications, such as cytokine inhibitors or non-steroidal anti-inflammatory drugs (NSAIDs), are underway.
- Neurotransmitter Modulation: Neurotransmitters such as serotonin, norepinephrine, and dopamine play key roles in pain processing and mood regulation. Drugs that target these neurotransmitter systems, such as selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs), may help modulate neuroinflammatory responses and improve symptoms of fibromyalgia.
- Lifestyle Interventions: Non-pharmacological approaches, including exercise, stress management techniques, and dietary modifications, may also exert anti-inflammatory effects and provide symptom relief in fibromyalgia. Regular physical activity has been shown to reduce inflammation and improve pain and function in individuals with fibromyalgia.
- Mind-Body Therapies: Mindfulness-based interventions, cognitive-behavioral therapy (CBT), and other mind-body techniques have demonstrated efficacy in reducing pain and improving coping skills in fibromyalgia. These approaches may exert their beneficial effects, in part, by modulating neuroinflammatory processes and restoring CNS homeostasis.
Challenges and Future Directions
While the emerging research on neuroinflammation in fibromyalgia offers promising avenues for treatment development, several challenges remain. The heterogeneity of fibromyalgia symptoms and the complex interplay of genetic, environmental, and psychosocial factors pose obstacles to identifying effective therapeutic targets. Furthermore, the lack of biomarkers for neuroinflammation in fibromyalgia complicates the diagnosis and monitoring of treatment response.

Moving forward, future research efforts should focus on elucidating the specific mechanisms driving neuroinflammation in fibromyalgia and identifying biomarkers that can guide personalized treatment approaches. Collaborative multidisciplinary approaches, integrating basic science, clinical research, and patient-centered outcomes, will be essential for advancing our understanding of neuroinflammation in fibromyalgia and translating this knowledge into effective treatments that improve the lives of individuals affected by this debilitating condition.
For any further queries, Plz visit drsmitagulatipainrelief.com