Myofascial pain syndrome (MPS) is a prevalent musculoskeletal disorder characterized by chronic pain and muscle tightness. This condition affects the fascia, the connective tissue that surrounds muscles, bones, and organs throughout the body. Understanding the underlying causes, symptoms, and management techniques of myofascial pain is crucial for those who suffer from it and for healthcare professionals who treat it. In this comprehensive guide, we delve into the intricate details of myofascial pain, providing insights into its nature, diagnosis, and effective management strategies.
What is Myofascial Pain?
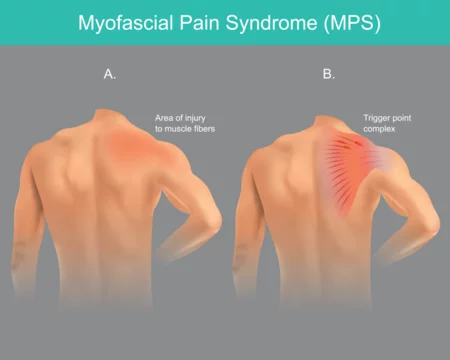
Myofascial pain arises from the dysfunction of the fascia, which can become tight, inflamed, or injured due to various factors such as overuse, trauma, poor posture, or stress. When the fascia becomes compromised, it can lead to the development of trigger points—localized areas of muscle spasm and tenderness. These trigger points can cause referred pain, meaning that discomfort is felt in areas distant from the actual trigger point itself. For example, a trigger point in the shoulder may manifest as pain in the neck or arm.
Causes and Triggers
Several factors contribute to the development of myofascial pain syndrome:
- Muscle Overuse: Repetitive motions or prolonged periods of muscle use, common in certain occupations or sports activities, can strain the muscles and fascia, leading to the formation of trigger points.
- Trauma or Injury: Acute injuries, such as falls, accidents, or sports-related injuries, can damage the muscle fibers and fascia, predisposing individuals to myofascial pain.
- Poor Posture: Maintaining improper posture for extended periods can place undue stress on certain muscle groups, causing them to become tight and prone to developing trigger points.
- Emotional Stress: Emotional tension and stress can contribute to muscle tension and trigger point formation, exacerbating myofascial pain symptoms.
- Medical Conditions: Certain medical conditions, such as fibromyalgia, arthritis, or temporomandibular joint disorder (TMJ), may increase the risk of developing myofascial pain syndrome.
Symptoms and Diagnosis
The hallmark symptom of myofascial pain is the presence of trigger points, which are tender nodules or bands within the muscle tissue. These trigger points can cause localized pain as well as referred pain in other areas of the body. Common symptoms of myofascial pain syndrome include:
- Muscle stiffness and tightness: Individuals with MPS often experience a sensation of stiffness or tightness in affected muscles, which may restrict their range of motion.
- Localized pain: Trigger points are typically tender to the touch and may elicit pain when pressure is applied.
- Referred pain: Discomfort originating from trigger points can radiate to other areas of the body, mimicking conditions such as headaches, jaw pain, or sciatica.
- Muscle weakness: Chronic muscle tension and pain can lead to muscle weakness and fatigue over time.
Diagnosing myofascial pain syndrome involves a thorough evaluation by a healthcare professional, typically a physician or physical therapist. The diagnostic process may include:
- Medical History: The healthcare provider will inquire about the patient’s medical history, including any previous injuries, underlying medical conditions, and lifestyle factors that may contribute to muscle pain.
- Physical Examination: A physical examination will be conducted to assess for the presence of trigger points, muscle tenderness, and areas of restricted movement.
- Trigger Point Identification: Palpation of the affected muscles helps identify trigger points and assess their tenderness and referral patterns.
- Imaging Studies: While not always necessary, imaging studies such as ultrasound or magnetic resonance imaging (MRI) may be ordered to rule out other potential causes of pain or to visualize muscle and fascial abnormalities.
Management Techniques
Effective management of myofascial pain syndrome involves a multimodal approach aimed at reducing pain, improving muscle function, and addressing underlying contributing factors. Treatment strategies may include:
- Manual Therapy: Techniques such as trigger point release, myofascial release, and massage therapy can help alleviate muscle tension, reduce trigger point activity, and improve tissue flexibility.
- Stretching and Strengthening Exercises: Targeted stretching and strengthening exercises prescribed by a physical therapist can help improve muscle flexibility, restore proper muscle balance, and prevent the recurrence of trigger points.
- Trigger Point Injections: Injection of local anesthetics, corticosteroids, or other medications directly into trigger points can help relieve pain and muscle tension.
- Dry Needling: This technique involves inserting thin needles into trigger points to stimulate a healing response and release muscle tension.
- Postural Correction: Education on proper posture and ergonomics is essential to prevent excessive strain on muscles and fascia. Individuals with myofascial pain syndrome should be encouraged to maintain good posture during daily activities and work-related tasks.
- Stress Management: Stress reduction techniques such as mindfulness meditation, deep breathing exercises, and progressive muscle relaxation can help alleviate emotional tension and reduce muscle tension.
- Medications: In some cases, medications such as nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, or tricyclic antidepressants may be prescribed to help manage pain, reduce inflammation, and improve sleep quality.
- Modalities: Heat therapy, cold therapy, ultrasound, and electrical stimulation are commonly used modalities to help relieve muscle pain, reduce inflammation, and promote tissue healing.
- Lifestyle Modifications: Adopting healthy lifestyle habits, including regular exercise, adequate sleep, and proper nutrition, can support overall musculoskeletal health and reduce the risk of myofascial pain recurrence.

Conclusion
Myofascial pain syndrome is a complex condition that can significantly impact an individual’s quality of life. By understanding the underlying mechanisms, recognizing common symptoms, and implementing effective management strategies, individuals with MPS can experience relief from pain and improve their overall musculoskeletal function. Collaboration between patients and healthcare providers is essential in developing personalized treatment plans tailored to address the unique needs of each individual. With proper education, support, and proactive management, individuals with myofascial pain syndrome can regain control of their symptoms and lead fulfilling, pain-free lives.
For any further queries, Plz visit drsmitagulatipainrelief.com



